
Vitamin C
 | |
|---|---|
 | |
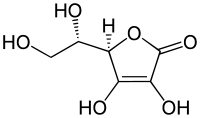
| Systematic (IUPAC) name | |
| 2-oxo-L-threo-hexono-1,4- lactone-2,3-enediol or (R)-3,4-dihydroxy-5-((S)- 1,2-dihydroxyethyl)furan-2(5H)-one | |
| Identifiers | |
| CAS number | 50-81-7 |
| ATC code | A11G |
| PubChem | CID 5785 |
| DrugBank | DB00126 |
| ChemSpider | 10189562 |
| UNII | PQ6CK8PD0R |
| Chemical data | |
| Formula | C6H8O6 |
| Mol. mass | 176.12 g/mole |
| SMILES | eMolecules & PubChem |
| Synonyms | L-ascorbic acid |
| Physical data | |
| Density | 1.694 g/cm³ |
| Melt. point | 190–192 °C (374–378 °F) decomposes |
| Boiling point | 553 °C (1027 °F) |
| Pharmacokinetic data | |
| Bioavailability | rapid & complete |
| Protein binding | negligible |
| Half-life | varies according to plasma concentration |
| Excretion | renal |
| Therapeutic considerations | |
| Pregnancy cat. | A |
| Legal status | general public availability |
| Routes | oral |
| | |
Vitamin C or L-ascorbic acid or L-ascorbate is an essential nutrient for humans and certain other animal species, in which it functions as a vitamin. In living organisms, ascorbate is an anti-oxidant, since it protects the body against oxidative stress.[1] It is also a cofactor in at least eight enzymatic reactions, including several collagen synthesis reactions that cause the most severe symptoms of scurvy when they are dysfunctional.[2] In animals, these reactions are especially important in wound-healing and in preventing bleeding from capillaries.
Ascorbate (an ion of ascorbic acid) is required for a range of essential metabolic reactions in all animals and plants. It is made internally by almost all organisms; notable mammalian group exceptions are most or all of the order chiroptera (bats), guinea pigs and one of the two major primate suborders, the Anthropoidea (Haplorrhini) (tarsiers, monkeys and apes, including human beings). Ascorbic acid is also not synthesized by guinea pigs, capybaras, and some species of birds and fish. All species that do not synthesize ascorbate require it in the diet. Deficiency in this vitamin causes the disease scurvy in humans.[3][4][5] It is also widely used as a food additive.[6]
Scurvy has been known since ancient times. People in many parts of the world assumed it was caused by a lack of fresh plant foods. The British Navy started giving sailors lime juice to prevent scurvy in 1795.[7] Ascorbic acid was finally isolated in 1932 and commercially "synthesized" (this included a fermentation step in bacteria) in 1934. The uses and recommended daily intake of vitamin C are matters of on-going debate, with RDI ranging from 45 to 95 mg/day. Proponents of megadosage propose from 200 mg to more than 2000 mg/day. The fraction of vitamin C in the diet that is absorbed and the rate at which the excess is eliminated from the body vary strongly with the dose. Large, randomized clinical trials on the effects of high doses on the general population have not been conducted.
Routine vitamin C supplementation does not reduce the incidence of the common cold in the general population.[8][9] In one study vitamin C supplementation significantly reduced the frequency of the common cold but without apparent effect on the duration or severity (however the authors of this research pointed out that the findings should be interpreted with caution).[10] As early as 1984 researchers knew that supplementation of drinking water with vitamin C increased the average life span of mice by as much as 20 percent.[11]
Biological significance
Further information: ascorbic acid
Vitamin C is purely the L-enantiomer of ascorbate; the opposite D-enantiomer has no physiological significance. Both forms are mirror images of the same molecular structure. When L-ascorbate, which is a strong reducing agent, carries out its reducing function, it is converted to its oxidized form, L-dehydroascorbate.[2] L-dehydroascorbate can then be reduced back to the active L-ascorbate form in the body by enzymes and glutathione.[12] During this process semidehydroascorbic acid radical is formed. Ascorbate free radical reacts poorly with oxygen, and thus, will not create a superoxide. Instead two semidehydroascorbate radicals will react and form one ascorbate and one dehydroascorbate. With the help of glutathione, dehydroxyascorbate is converted back to ascorbate.[13] The presence of glutathione is crucial since it spares ascorbate and improves antioxidant capacity of blood.[14] Without it dehydroxyascorbate could not convert back to ascorbate.
L-Ascorbate is a weak sugar acid structurally related to glucose that naturally occurs attached either to a hydrogen ion, forming ascorbic acid, or to a metal ion, forming a mineral ascorbate.
[edit] Biosynthesis and species-specific synthetic ability
Model of a vitamin C molecule. Black is carbon, red is oxygen, and white is hydrogen
The vast majority of animals and plants are able to synthesize their own vitamin C, through a sequence of four enzyme-driven steps, which convert glucose to vitamin C.[2] The glucose needed to produce ascorbate in the liver (in mammals and perching birds) is extracted from glycogen; ascorbate synthesis is a glycogenolysis-dependent process.[15] In reptiles and birds the biosynthesis is carried out in the kidneys.
Among the animals that have lost the ability to synthesise vitamin C are simians and tarsiers, which together make up one of two major primate suborders, the anthropoidea, also called haplorrhini. This group includes humans. The other more primitive primates (strepsirrhini) retained the ability to make vitamin C, so this loss probably occurred in a common ancestor of the haplorrhini. Synthetic ability has been lost in a number of species (perhaps all species) in the small rodent family caviidae that includes guinea pigs and capybaras, but retained in other rodents (rats and mice do not need vitamin C in their diet, for example). A number of species of passerine birds also lost the ability, but not all of them, and those that have lost it are not clearly related; there is some evidence that the ability was lost separately a number of times in birds.[16] All tested families of bats, including major insect and fruit-eating bat families have lost the ability to make vitamin C, and this loss may derive from a common bat ancestor, as a single mutation.[17]
These animals all lack the L-gulonolactone oxidase (GULO) enzyme, which is required in the last step of vitamin C synthesis, because they have a defective form of the gene for the enzyme (Pseudogene ΨGULO).[18] The remains of this non-functional gene with many mutations are, however, still present in the genome of the guinea pigs and in primates, including humans.[19][20] Some of these species (including humans) are able to make do with the lower levels available from their diets by recycling oxidised vitamin C.[21]
Most simians consume the vitamin in amounts 10 to 20 times higher than that recommended by governments for humans.[22] This discrepancy constitutes much of the basis of the controversy on current recommended dietary allowances. It is countered by arguments that humans are very good at conserving dietary vitamin C, and are able to maintain blood levels of vitamin C comparable with other simians, on a far smaller dietary intake.
An adult goat, a typical example of a vitamin C-producing animal, will manufacture more than 13 g of vitamin C per day in normal health and the biosynthesis will increase "manyfold under stress".[23] Trauma or injury has also been demonstrated to use up large quantities of vitamin C in humans.[24] Some microorganisms such as the yeast Saccharomyces cerevisiae have been shown to be able to synthesize vitamin C from simple sugars.[25][26]
[edit] Vitamin C in evolution
Venturi and Venturi[27][28] suggested that the antioxidant action of ascorbic acid developed first in the plant kingdom when, about 500 million years ago (Mya), plants began to adapt to antioxidant-mineral-deficient fresh-waters of estuaries. Some biologists suggested that many vertebrates had developed their metabolic adaptive strategies in estuary environment.[29] In this theory, some 400-300 Mya, when living plants and animals first began the move from the sea to rivers and land, environmental iodine deficiency was a challenge to the evolution of terrestrial life.[30] In plants, animals and fishes, the terrestrial diet became deficient in many essential antioxidant marine micronutrients, including iodine, selenium, zinc, copper, manganese, iron, etc. Freshwater algae and terrestrial plants, in replacement of marine antioxidants, slowly optimized the production of other endogenous antioxidants such as ascorbic acid, polyphenols, carotenoids, tocopherols etc., some of which became essential “vitamins” in the diet of terrestrial animals (vitamins C, A, E, etc.).
Ascorbic acid or vitamin C is a common enzymatic cofactor in mammals used in the synthesis of collagen. Ascorbate is a powerful reducing agent capable of rapidly scavenging a number of reactive oxygen species (ROS). Freshwater teleost fishes also require dietary vitamin C in their diet or they will get scurvy. The most widely recognized symptoms of vitamin C deficiency in fishes are scoliosis, lordosis and dark skin coloration. Freshwater salmonids also show impaired collagen formation, internal/fin haemorrhage, spinal curvature and increased mortality. If these fishes are housed in seawater with algae and phytoplankton, then vitamin supplementation seems to be less important, it is presumed because of the availability of other, more ancient, antioxidants in natural marine environment.[31]
Some scientists have suggested that loss of the vitamin C biosynthesis pathway may have played a role in the sequence of rapid evolutionary changes that led to hominids and the emergence of human beings.[32][33][34] However, the loss of ability to make vitamin C in simians must have occurred much farther back in evolutionary history than the emergence of humans or even apes, since it evidently occurred rather soon after the appearance of the first primates, yet sometime after the split of early primates into its two major suborders haplorrhini (which cannot make vitamin C) and its sister suborder of non-tarsier prosimians, the strepsirrhini ("wet-nosed" primates), which retained the ability to make vitamin C.[35] According to molecular clock dating, these two suborder primate branches parted ways about 63 to 60 Mya[36] Approximately three to five million years later (58 Mya), only a short time afterward from an evolutionary perspective, the infraorder Tarsiiformes, whose only remaining family is that of the tarsier (Tarsiidae), branched off from the other haplorrhines.[37][38] Since tarsiers also cannot make vitamin C, this implies the mutation had already occurred, and thus must have occurred between these two marker points (63 to 58 Mya).
It has been noted that the loss of the ability to synthesize ascorbate strikingly parallels the evolutionary loss of the ability to break down uric acid, also a characteristic of primates. Uric acid and ascorbate are both strong reducing agents. This has led to the suggestion that, in higher primates, uric acid has taken over some of the functions of ascorbate.[39]
[edit] Absorption, transport, and disposal
Ascorbic acid is absorbed in the body by both active transport and simple diffusion. Sodium-Dependent Active Transport - Sodium-Ascorbate Co-Transporters (SVCTs) and Hexose transporters (GLUTs) - are the two transporters required for absorption. SVCT1 and SVCT2 imported the reduced form of ascorbate across plasma membrane.[40] GLUT1 and GLUT3 are the two glucose transporters, and transfer only dehydroascorbic acid form of Vitamin C.[41] Although dehydroascorbic acid is absorbed in higher rate than ascorbate, the amount of dehydroascorbic acid found in plasma and tissues under normal conditions is low, as cells rapidly reduce dehydroascorbic acid to ascorbate.[42][43] Thus, SVCTs appear to be the predominant system for vitamin C transport in the body.
SVCT2 is involved in vitamin C transport in almost every tissue,[40] the notable exception being red blood cells, which lose SVCT proteins during maturation.[44] "SVCT2 knockout" animals genetically engineered to lack this functional gene, die shortly after birth,[45] suggesting that SVCT2-mediated vitamin C transport is necessary for life.
With regular intake the absorption rate varies between 70 to 95%. However, the degree of absorption decreases as intake increases. At high intake (12g), fractional human absorption of ascorbic acid may be as low as 16%; at low intake (<20 mg) the absorption rate can reach up to 98%.[46] Ascorbate concentrations over renal re-absorption threshold pass freely into the urine and are excreted. At high dietary doses (corresponding to several hundred mg/day in humans) ascorbate is accumulated in the body until the plasma levels reach the renal resorption threshold, which is about 1.5 mg/dL in men and 1.3 mg/dL in women. Concentrations in the plasma larger than this value (thought to represent body saturation) are rapidly excreted in the urine with a half-life of about 30 minutes. Concentrations less than this threshold amount are actively retained by the kidneys, and the excretion half-life for the remainder of the vitamin C store in the body thus increases greatly, with the half-life lengthening as the body stores are depleted. This half-life rises until it is as long as 83 days by the onset of the first symptoms of scurvy.[47]
Although the body's maximal store of vitamin C is largely determined by the renal threshold for blood, there are many tissues that maintain vitamin C concentrations far higher than in blood. Biological tissues that accumulate over 100 times the level in blood plasma of vitamin C are the adrenal glands, pituitary, thymus, corpus luteum, and retina.[48] Those with 10 to 50 times the concentration present in blood plasma include the brain, spleen, lung, testicle, lymph nodes, liver, thyroid, small intestinal mucosa, leukocytes, pancreas, kidney and salivary glands.
Ascorbic acid can be oxidized (broken down) in the human body by the enzyme L-ascorbate oxidase. Ascorbate that is not directly excreted in the urine as a result of body saturation or destroyed in other body metabolism is oxidized by this enzyme and removed.
[edit] Deficiency
Main article: Scurvy
Scurvy is an avitaminosis resulting from lack of vitamin C, since without this vitamin, the synthesised collagen is too unstable to perform its function. Scurvy leads to the formation of brown spots on the skin, spongy gums, and bleeding from all mucous membranes. The spots are most abundant on the thighs and legs, and a person with the ailment looks pale, feels depressed, and is partially immobilized. In advanced scurvy there are open, suppurating wounds and loss of teeth and, eventually, death. The human body can store only a certain amount of vitamin C,[49] and so the body stores are depleted if fresh supplies are not consumed. The time frame for onset of symptoms of scurvy in unstressed adults switched to a completely vitamin C free diet, however, may range from one month to more than six months, depending on previous loading of vitamin C (see below).
It has been shown that smokers who have diets poor in vitamin C are at a higher risk of lung-borne diseases than those smokers who have higher concentrations of vitamin C in the blood.[50]
Nobel prize winner Linus Pauling and Dr. G. C. Willis have asserted that chronic long term low blood levels of vitamin C (chronic scurvy) is a cause of atherosclerosis.[51]
Western societies generally consume far more than sufficient Vitamin C to prevent scurvy. In 2004, a Canadian Community health survey reported that Canadians of 19 years and above have intakes of vitamin C from food of 133 mg/d for males and 120 mg/d for females,[52] that is higher than the RDA recommendation.
Notable human dietary studies of experimentally-induced scurvy have been conducted on conscientious objectors during WW II in Britain, and on Iowa state prisoner "volunteers" in the late 1960s. These studies both found that all obvious symptoms of scurvy previously induced by an experimental scorbutic diet with extremely low vitamin C content, could be completely reversed by additional vitamin C supplementation of only 10 mg a day. In these experiments, there was no clinical difference noted between men given 70 mg vitamin C per day (which produced blood level of vitamin C of about 0.55 mg/dl, about 1/3 of tissue saturation levels), and those given 10 mg per day. Men in the prison study developed the first signs of scurvy about 4 weeks after starting the vitamin C free diet, whereas in the British study, six to eight months were required, possibly due to the pre-loading of this group with a 70 mg/day supplement for six weeks before the scorbutic diet was fed.[53]
Men in both studies on a diet devoid, or nearly devoid, of vitamin C had blood levels of vitamin C too low to be accurately measured when they developed signs of scurvy, and in the Iowa study, at this time were estimated (by labeled vitamin C dilution) to have a body pool of less than 300 mg, with daily turnover of only 2.5 mg/day, implying a instantaneous half-life of 83 days by this time (elimination constant of 4 months).[54]
Moderately higher blood levels of vitamin C measured in healthy persons have been found to be prospectively correlated with decreased risk of cardiovascular disease and ischaemic heart disease, and an increase life expectancy. The same study found an inverse relationship between blood vitamin C levels and cancer risk in men, but not women. An increase in blood level of 20 micromol/L of vitamin C (about 0.35 mg/dL, and representing a theoretical additional 50 grams of fruit and vegetables per day) was found epidemiologically to reduce the all-cause risk of mortality, four years after measuring it, by about 20%.[55] However, because this was not an intervention study, causation could not be proven, and vitamin C blood levels acting as a proxy marker for other differences between the groups could not be ruled out. However, the four-year long and prospective nature of the study did rule out proxy effect from any vitamin-C lowering effects of immediately-terminal illness, or near-end-of-life poor health.
Studies with much higher doses of vitamin C, usually between 200 and 6000 mg, for the treatment of infections and wounds have shown inconsistent results.[56] While combinations of antioxidants seem to improve wound healing,[57]
[edit] History of human understanding
James Lind, a British Royal Navy surgeon who, in 1747, identified that a quality in fruit prevented the disease of scurvy in what was the first recorded controlled experiment.
The need to include fresh plant food or raw animal flesh in the diet to prevent disease was known from ancient times. Native people living in marginal areas incorporated this into their medicinal lore. For example, spruce needles were used in temperate zones in infusions, or the leaves from species of drought-resistant trees in desert areas. In 1536, the French explorer Jacques Cartier, exploring the St. Lawrence River, used the local natives' knowledge to save his men who were dying of scurvy. He boiled the needles of the arbor vitae tree to make a tea that was later shown to contain 50 mg of vitamin C per 100 grams.[58][59]
Throughout history, the benefit of plant food to survive long sea voyages has been occasionally recommended by authorities. John Woodall, the first appointed surgeon to the British East India Company, recommended the preventive and curative use of lemon juice in his book, The Surgeon's Mate, in 1617. The Dutch writer, Johann Bachstrom, in 1734, gave the firm opinion that "scurvy is solely owing to a total abstinence from fresh vegetable food, and greens, which is alone the primary cause of the disease."[60]
In the early days of long sea voyages, scurvy killed more sailors than did warfare, accidents, and other causes.[61] For instance, in 1499, Vasco da Gama lost two thirds of his crew while making his way to India; and in 1520, Magellan lost more than 80 per cent while crossing the Pacific – all mainly to scurvy.[62]
While the earliest documented case of scurvy was described by Hippocrates around the year 400 BC, the first attempt to give scientific basis for the cause of this disease was by a ship's surgeon in the British Royal Navy, James Lind. Scurvy was common among those with poor access to fresh fruit and vegetables, such as remote, isolated sailors and soldiers. While at sea in May 1747, Lind provided some crew members with two oranges and one lemon per day, in addition to normal rations, while others continued on cider, vinegar, sulfuric acid or seawater, along with their normal rations. In the history of science, this is considered to be the first occurrence of a controlled experiment comparing results on two populations of a factor applied to one group only with all other factors the same. The results conclusively showed that citrus fruits prevented the disease. Lind published his work in 1753 in his Treatise on the Scurvy.[63]
Citrus fruits were one of the first sources of vitamin C available to ships' surgeons.
Lind's work was slow to be noticed, partly because his Treatise was not published until six years after his study, and also because he recommended a lemon juice extract known as rob.[64] Fresh fruit was very expensive to keep on board, whereas boiling it down to juice allowed easy storage but destroyed the vitamin (especially if boiled in copper kettles).[65] Ship captains concluded wrongly that Lind's other suggestions were ineffective because those juices failed to prevent or cure scurvy.
It was 1795 before the British navy adopted lemons or lime as standard issue at sea. Limes were more popular, as they could be found in British West Indian Colonies, unlike lemons, which were not found in British Dominions, and were therefore more expensive. This practice led to the American use of the nickname "limey" to refer to the British. Captain James Cook had previously demonstrated and proven the principle of the advantages of carrying "Sour krout" on board, by taking his crews to the Hawaiian Islands and beyond without losing any of his men to scurvy.[66] For this otherwise unheard of feat, the British Admiralty awarded him a medal.
The name antiscorbutic was used in the eighteenth and nineteenth centuries as general term for those foods known to prevent scurvy, even though there was no understanding of the reason for this. These foods included but were not limited to: lemons, limes, and oranges; sauerkraut, cabbage, malt, and portable soup.[67]
Even before the antiscorbutic substance was identified, there were indications that it was present in amounts sufficient to prevent scurvy, in nearly all fresh (uncooked and uncured) foods, including raw animal-derived foods. In 1928, the Arctic anthropologist Vilhjalmur Stefansson attempted to prove his theory of how the Eskimos are able to avoid scurvy with almost no plant food in their diet, despite the disease's striking European Arctic explorers living on similar high-cooked-meat diets. Stefansson theorised that the natives get their vitamin C from fresh meat that is minimally cooked. Starting in February 1928, for one year he and a colleague lived on an exclusively minimally-cooked meat diet while under medical supervision; they remained healthy. Later studies done after vitamin C could be quantified in mostly-raw traditional food diets of the Yukon, Inuit, and Métís of the Northern Canada, showed that their daily intake of vitamin C averaged between 52 and 62 mg/day, an amount approximately the dietary reference intake (DRI), even at times of the year when little plant-based food were eaten.[68]
[edit] Discovery
Albert Szent-Györgyi, pictured here in 1948, was awarded the 1937 Nobel Prize in Medicine "for his discoveries in connection with the biological combustion processes, with special reference to vitamin C and the catalysis of fumaric acid".
In 1907, the needed biological-assay model to isolate and identify the antiscorbutic factor was discovered. Axel Holst and Theodor Frølich, two Norwegian physicians studying shipboard beriberi contracted aboard ship's crews in the Norwegian Fishing Fleet, wanted a small test mammal to substitute for the pigeons then used in beriberi research. They fed guinea pigs their test diet of grains and flour, which had earlier produced beriberi in their pigeons, and were surprised when classic scurvy resulted instead. This was a serendipitous choice of model. Until that time, scurvy had not been observed in any organism apart from humans, and had been considered an exclusively human disease. (Pigeons, as seed-eating birds, were also later found to make their own vitamin C.) Holst and Frølich found they could cure the disease in guinea pigs with the addition of various fresh foods and extracts. This discovery of a clean animal experimental model for scurvy, made even before the essential idea of vitamins in foods had even been put forward, has been called the single most important piece of vitamin C research.[69]
In 1912, the Polish-American biochemist Casimir Funk, while researching beriberi in pigeons, developed the concept of vitamins to refer to the non-mineral micro-nutrients that are essential to health. The name is a blend of "vital", due to the vital biochemical role they play, and "amines" because Funk thought that all these materials were chemical amines. Although the "e" was dropped after skepticism that all these compounds were amines, the word vitamin remained as a generic name for them. One of the vitamins was thought to be the anti-scorbutic factor in foods discovered by Holst and Frølich. In 1928, this vitamin was referred to as "water-soluble C," although its chemical structure had still not been determined. [70]
From 1928 to 1933, the Hungarian research team of Joseph L. Svirbely and Albert Szent-Györgyi and the American worker Charles Glen King, first identified the anti-scorbutic factor, calling it "ascorbic acid" for its vitamin activity. Szent-Györgyi had isolated the chemical hexuronic acid from animal adrenal glands at the Mayo clinic, and suspected it to be the antiscorbutic factor, but could not prove it without a biological assay. At the same time, for five years, King's laboratory at the University of Pittsburgh had been trying to isolate the antiscorbutic factor in lemon juice, using the model of scorbutic guinea pigs, which developed scurvy when not fed fresh foods, but were cured by lemon juice. They had also considered hexuronic acid, but had been put off the trail when a coworker made the explicit (and mistaken) experimental claim that this substance was not the antiscorbutic substance.
Finally, in late 1931, Szent-Györgyi gave Svirbely, a former worker in King's lab who had recently joined Szent-Györgyi's lab, the last of this hexuronic acid, with the suggestion that it might be the anti-scorbutic factor. By the spring of 1932, King's laboratory had proven this, but published the result without giving Szent-Györgyi credit for it, leading to a bitter dispute over priority claims (in reality it had taken a teamwork effort by both groups, since Szent-Györgyi was unwilling to do the difficult and messy animal studies). By 1932, Szent-Györgyi's group had discovered that paprika peppers, a common spice in the Hungarian diet, was a rich source of hexuronic acid, the antiscorbutic factor, by then named ascorbic acid, in honor of its activity against scurvy.[71] Ascorbic acid turned out not to be an amine, or even to contain any nitrogen.
For his accomplishment, Szent-Györgyi was alone awarded the 1937 Nobel Prize in Medicine "for his discoveries in connection with the biological combustion processes, with special reference to vitamin C and the catalysis of fumaric acid".[72]
Between 1933 and 1934, the British chemists Sir Walter Norman Haworth and Sir Edmund Hirst and, independently, the Polish chemist Tadeus Reichstein, succeeded in synthesizing the vitamin, making it the first to be artificially produced. This made possible the cheap mass-production of what was by then known as vitamin C. Only Haworth was awarded the 1937 Nobel Prize in Chemistry for this work, but the Reichstein process, a combined chemical and bacterial fermentation sequence still used today to produce vitamin C, retained Reichstein's name.[73][74] In 1934 Hoffmann–La Roche, which bought the Reichstein process patent, became the first pharmaceutical company to mass-produce and market synthetic vitamin C, under the brand name of Redoxon.[75]
In 1957, the American J.J. Burns showed that the reason some mammals are susceptible to scurvy is the inability of their liver to produce the active enzyme L-gulonolactone oxidase, which is the last of the chain of four enzymes that synthesize vitamin C.[76][77] American biochemist Irwin Stone was the first to exploit vitamin C for its food preservative properties. He later developed the theory that humans possess a mutated form of the L-gulonolactone oxidase coding gene.[78]
In 2008, researchers at the University of Montpellier discovered that, in humans and other primates, the red blood cells have evolved a mechanism to more efficiently utilize the vitamin C present in the body by recycling oxidized L-dehydroascorbic acid (DHA) back into ascorbic acid, which can be reused by the body. The mechanism was not found to be present in mammals that synthesize their own vitamin C.[21]
[edit] Physiological function in mammals
In humans, vitamin C is essential to a healthy diet as well as being a highly effective antioxidant, acting to lessen oxidative stress; a substrate for ascorbate peroxidase in plants (APX is plant specific enzyme);[5] and an enzyme cofactor for the biosynthesis of many important biochemicals. Vitamin C acts as an electron donor for important enzymes:[79]
[edit] Collagen, carnitine, and tyrosine synthesis, and microsomal metabolism
Ascorbic acid performs numerous physiological functions in the human body. These functions include the synthesis of collagen, carnitine, and neurotransmitters, the synthesis and catabolism of tyrosine, and the metabolism of microsome.[14] During biosynthesis ascorbate acts as a reducing agent, donating electrons and preventing oxidation to keep iron and copper atoms in their reduced states.
Vitamin C acts as an electron donor for eight different enzymes:[79]
* Three enzymes participate in collagen hydroxylation.[80][81][82] These reactions add hydroxyl groups to the amino acids proline or lysine in the collagen molecule via prolyl hydroxylase and lysyl hydroxylase, both requiring vitamin C as a cofactor. Hydroxylation allows the collagen molecule to assume its triple helix structure and making vitamin C essential to the development and maintenance of scar tissue, blood vessels, and cartilage.[49]
* Two enzymes are necessary for synthesis of carnitine.[83][84] Carnitine is essential for the transport of fatty acids into mitochondria for ATP generation.
* The remaining three enzymes have the following functions in common, but have other functions as well:
o dopamine beta hydroxylase participates in the biosynthesis of norepinephrine from dopamine.[85][86]
o another enzyme adds amide groups to peptide hormones, greatly increasing their stability.[87][88]
o one modulates tyrosine metabolism.[89][90]
[edit] Antioxidant
Ascorbic acid is well known for its antioxidant activity, acting as a reducing agent to reverse oxidation in liquids. When there are more free radicals (reactive oxygen species, ROS) in the human body than antioxidants, the condition is called oxidative stress,[91] and has an impact on cardiovascular disease, hypertension, chronic inflammatory diseases, diabetes[92][93][94][95] as well as on critically ill patients and individuals with severe burns.[91] Individuals experiencing oxidative stress have ascorbate blood levels lower than 45 µmol/L, compared to healthy individual who range between 61.4-80 µmol/L.[96]
It is not yet certain whether vitamin C and antioxidants in general prevent oxidative stress-related diseases and promote health. Clinical studies regarding the effects of vitamin C supplementation on lipoproteins and cholesterol have found that vitamin C supplementation does not improve disease markers in the blood.[97][98] Vitamin C may contribute to decreased risk of cardiovascular disease and strokes through a small reduction in systolic blood pressure,[99] and was also found to both increase ascorbic acid levels and reduce levels of resistin serum,[100] another likely determinant of oxidative stress and cardiovascular risk. However, so far there is no consensus that vitamin C intake has an impact on cardiovascular risks in general, and an array of studies found negative results.[101] Meta-analysis of a large number of studies on antioxidants, including vitamin C supplementation, found no relationship between vitamin C and mortality. Thus vitamin C does not appear to help people live longer.[102]
[edit] Pro-oxidant
Ascorbic acid behaves not only as an antioxidant but also as a pro-oxidant.[91] Ascorbic acid has been shown to reduce transition metals, such as cupric ions (Cu2+), to cuprous (Cu1+), and ferric ions (Fe3+) to ferrous (Fe2+) during conversion from ascorbate to dehydroascorbate in vitro.[103] This reaction can generate superoxide and other ROS. However, in the body, free transition elements are unlikely to be present while iron and copper are bound to diverse proteins[91] and the intravenous use of vitamin C does not appear to increase pro-oxidant activity.[104] Thus, ascorbate as a pro-oxidant is unlikely to convert metals to create ROS in vivo. However, vitamin C supplementation has been associated with increased DNA damage in the lymphocytes of healthy volunteers.[105]
[edit] Immune system
Some advertisements claim that Vitamin C "supports" or is "important" for immune system function. Vitamin C deficiency is detrimental to immune function, resulting in reduced resistance to some pathogens. Routine supplementation is not indicated in the general population, though there is some evidence that it reduces symptom severity but not incidence of the common cold. Effects are most pronounced in cases of physical strain or insufficient dietary intake.[8][106]
[edit] Antihistamine
Vitamin C is a natural antihistamine. It both prevents histamine release and increases the detoxification of histamine. A 1992 study found that taking 2 grams vitamin C daily lowered blood histamine levels 38 percent in healthy adults in just one week.[107] It has also been noted that low concentrations of serum vitamin C has been correlated with increased serum histamine levels.[citation needed]
[edit] Physiologic function in plants
Ascorbic acid is associated with chloroplasts and apparently plays a role in ameliorating the oxidative stress of photosynthesis. In addition, it has a number of other roles in cell division and protein modification. Plants appear to be able to make ascorbate by at least one other biochemical route that is different from the major route in animals, although precise details remain unknown.[108]
[edit] Daily requirements
The North American Dietary Reference Intake recommends 90 milligrams per day and no more than 2 grams (2,000 milligrams) per day.[109] Other related species sharing the same inability to produce vitamin C and requiring exogenous vitamin C consume 20 to 80 times this reference intake.[110] There is continuing debate within the scientific community over the best dose schedule (the amount and frequency of intake) of vitamin C for maintaining optimal health in humans.[111] It is generally agreed that a balanced diet without supplementation contains enough vitamin C to prevent scurvy in an average healthy adult, while those who are pregnant, smoke tobacco, or are under stress require slightly more.[109]
High doses (thousands of milligrams) may result in diarrhea in healthy adults, as a result of the osmotic water-retaining effect of the unabsorbed portion in the gastrointestinal tract (similar to cathartic osmotic laxatives). Proponents of orthomolecular medicine[112] claim the onset of diarrhea to be an indication of where the body’s true vitamin C requirement lies, though this has not been clinically verified.
United States vitamin C recommendations[109]
Recommended Dietary Allowance (adult male) 90 mg per day
Recommended Dietary Allowance (adult female) 75 mg per day
Tolerable Upper Intake Level (adult male) 2,000 mg per day
Tolerable Upper Intake Level (adult female) 2,000 mg per day
[edit] Government recommended intakes
Recommendations for vitamin C intake have been set by various national agencies:
* 40 milligrams per day: the United Kingdom's Food Standards Agency[3]
* 45 milligrams per day: the World Health Organization[113]
* 90 mg/day (males) and 75 mg/day (females): Health Canada 2007[114]
* 60–95 milligrams per day: United States' National Academy of Sciences.[109]
The United States defined Tolerable Upper Intake Level for a 25-year-old male is 2,000 milligrams per day.
[edit] Alternative recommendations on intakes
Some independent researchers have calculated the amount needed for an adult human to achieve similar blood serum levels as vitamin C synthesising mammals as follows:
* 400 milligrams per day: the Linus Pauling Institute.[115]
* 500 milligrams per 12 hours: Professor Roc Ordman, from research into biological free radicals.[116]
* 4,000 milligrams per day: Patrick Holford & Jerome Burne.[117]
* 6,000–12,000 milligrams per day: Thomas E. Levy, Colorado Integrative Medical Centre.[118]
* 6,000–18,000 milligrams per day: Linus Pauling's personal use.[119]
[edit] Therapeutic uses
Vitamin C functions as an antioxidant and is necessary for the treatment and prevention of scurvy, though in nearly all cases dietary intake is adequate to prevent deficiency and supplementation is not necessary.[120][121][122][123][124][125]
Vitamin C may also be useful in lowering serum uric acid levels resulting in a correspondingly lower incidence of gout,[126] and an oxidized version that can cross the blood-brain barrier may reduce neurological deficits and mortality following a stroke.[127] There is suggestive evidence vitamin C may be useful in the treatment of pneumonia.[128]
Vitamin C's effect on the common cold has been extensively researched and shown not to have so much effect as was supposed.[8][9]
[edit] Vitamin C megadosage
Main article: Vitamin C megadosage
Several individuals and organizations advocate large doses of vitamin C,[129] although large, randomized clinical trials on the effects of high doses on the general population have never taken place. Individuals who have recommended intake well in excess of the current Dietary Reference Intake (DRI) include Robert Cathcart, Ewan Cameron, Steve Hickey, Irwin Stone, Matthias Rath and Linus Pauling. Arguments for megadosage are based on the diets of closely related apes and the likely diet of pre-historical humans, and that most mammals synthesize vitamin C rather than relying on dietary intake. Stone[130] and Pauling[131] believed that the optimum daily requirement of vitamin C is around 2,300 milligrams for a human requiring 2,500 kcal a day. Pauling criticized the established RDA as sufficient to prevent scurvy, but not necessarily the dosage for optimal health.[119]
Though vitamin C has been promoted as useful in the treatment of a variety of conditions, these uses are poorly supported by the evidence and sometimes contraindicated.[132][133][134][135]
[edit] Testing for ascorbate levels in the body
Simple tests use dichlorophenolindophenol, a redox indicator, to measure the levels of vitamin C in the urine and in serum or blood plasma. However these reflect recent dietary intake rather than the level of vitamin C in body stores.[2] Reverse phase high performance liquid chromatography is used for determining the storage levels of vitamin C within lymphocytes and tissue. It has been observed that while serum or blood plasma levels follow the circadian rhythm or short term dietary changes, those within tissues themselves are more stable and give a better view of the availability of ascorbate within the organism. However, very few hospital laboratories are adequately equipped and trained to carry out such detailed analyses, and require samples to be analyzed in specialized laboratories.[136][137]
[edit] Adverse effects
[edit] Common side-effects
Relatively large doses of vitamin C may cause indigestion, particularly when taken on an empty stomach. When taken in large doses, vitamin C causes diarrhea in healthy subjects. In one trial in 1936, doses up to 6 grams of ascorbic acid were given to 29 infants, 93 children of preschool and school age, and 20 adults for more than 1400 days. With the higher doses, toxic manifestations were observed in five adults and four infants. The signs and symptoms in adults were nausea, vomiting, diarrhea, flushing of the face, headache, fatigue and disturbed sleep. The main toxic reactions in the infants were skin rashes.[138]
[edit] Possible side-effects
As vitamin C enhances iron absorption,[139] iron poisoning can become an issue to people with rare iron overload disorders, such as haemochromatosis. A genetic condition that results in inadequate levels of the enzyme glucose-6-phosphate dehydrogenase (G6PD) can cause sufferers to develop hemolytic anemia after ingesting specific oxidizing substances, such as very large dosages of vitamin C.[140]
There is a longstanding belief among the mainstream medical community that vitamin C causes kidney stones, which is based on little science.[141] Although recent studies have found a relationship,[142] a clear link between excess ascorbic acid intake and kidney stone formation has not been generally established.[143] Some case reports exist for a link between patients with oxalate deposits and a history of high-dose vitamin C usage.[144]
In a study conducted on rats, during the first month of pregnancy, high doses of vitamin C may suppress the production of progesterone from the corpus luteum.[145] Progesterone, necessary for the maintenance of a pregnancy, is produced by the corpus luteum for the first few weeks, until the placenta is developed enough to produce its own source. By blocking this function of the corpus luteum, high doses of vitamin C (1000+ mg) are theorized to induce an early miscarriage. In a group of spontaneously aborting women at the end of the first trimester, the mean values of vitamin C were significantly higher in the aborting group. However, the authors do state: 'This could not be interpreted as an evidence of casual association.'[146] However, in a previous study of 79 women with threatened, previous spontaneous, or habitual abortion, Javert and Stander (1943) had 91% success with 33 patients who received vitamin C together with bioflavonoids and vitamin K (only three abortions), whereas all of the 46 patients who did not receive the vitamins aborted.[147]
A study in rats and humans suggested that adding Vitamin C supplements to an exercise training program lowered the expected effect of training on VO2Max. Although the results in humans were not statistically significant, this study is often cited as evidence that high doses of Vitamin C have an adverse effect on exercise performance. In rats, it was shown that the additional Vitamin C resulted in lowered mitochondria production.[148] Since rats are able to produce all of their needed Vitamin C, however, it is questionable whether they offer a relevant model of human physiological processes in this regard.
A cancer-causing mechanism of hexavalent chromium may be triggered by vitamin C.[149]
[edit] Chance of overdose
Vitamin C is water soluble, with dietary excesses not absorbed, and excesses in the blood rapidly excreted in the urine. It exhibits remarkably low toxicity. The LD50 (the dose that will kill 50% of a population) in rats is generally accepted to be 11.9 grams per kilogram of body weight when given by forced gavage (orally). The mechanism of death from such doses (1.2% of body weight, or 1.8 lbs for a 150 lb human) is unknown, but may be more mechanical than chemical.[65] The LD50 in humans remains unknown, given lack of any accidental or intentional poisoning death data. However, as with all substances tested in this way, the rat LD50 is taken as a guide to its toxicity in humans.
[edit] Natural and synthetic dietary sources
Rose hips are a particularly rich source of vitamin C
The richest natural sources are fruits and vegetables, and of those, the Kakadu plum and the camu camu fruit contain the highest concentration of the vitamin. It is also present in some cuts of meat, especially liver. Vitamin C is the most widely taken nutritional supplement and is available in a variety of forms, including tablets, drink mixes, crystals in capsules or naked crystals.
Vitamin C is absorbed by the intestines using a sodium-ion dependent channel. It is transported through the intestine via both glucose-sensitive and glucose-insensitive mechanisms. The presence of large quantities of sugar either in the intestines or in the blood can slow absorption.[150]
[edit] Plant sources
While plants are generally a good source of vitamin C, the amount in foods of plant origin depends on the precise variety of the plant, soil condition, climate where it grew, length of time since it was picked, storage conditions, and method of preparation.[151]
The following table is approximate and shows the relative abundance in different raw plant sources.[152][153][154] As some plants were analyzed fresh while others were dried (thus, artifactually increasing concentration of individual constituents like vitamin C), the data are subject to potential variation and difficulties for comparison. The amount is given in milligrams per 100 grams of fruit or vegetable and is a rounded average from multiple authoritative sources:
Plant source Amount
(mg / 100g)
Kakadu plum 3100
Camu Camu 2800
Rose hip 2000
Acerola 1600
Seabuckthorn 695
Jujube 500
Indian gooseberry 445
Baobab 400
Hot Chillis - Green 244
Blackcurrant 200
Red pepper 190
Hot Chillis - Red 144
Parsley 130
Guava 100
Kiwifruit 90
Broccoli 90
Loganberry 80
Redcurrant 80
Brussels sprouts 80
Wolfberry (Goji) 73 †
Lychee 70
Cloudberry 60
Elderberry 60
Persimmon 60
† average of 3 sources; dried
Plant source Amount
(mg / 100g)
Papaya 60
Strawberry 60
Orange 50
Kale 41
Lemon 40
Melon, cantaloupe 40
Cauliflower 40
Garlic 31
Grapefruit 30
Raspberry 30
Tangerine 30
Mandarin orange 30
Passion fruit 30
Spinach 30
Cabbage raw green 30
Lime 30
Mango 28
Blackberry 21
Potato 20
Melon, honeydew 20
Cranberry 13
Tomato 10
Blueberry 10
Pineapple 10
Pawpaw 10
Plant source Amount
(mg / 100g)
Grape 10
Apricot 10
Plum 10
Watermelon 10
Banana 9
Carrot 9
Avocado 8
Crabapple 8
Persimmon - fresh 7
Cherry 7
Peach 7
Apple 6
Asparagus 6
Beetroot 5
Chokecherry 5
Pear 4
Lettuce 4
Cucumber 3
Eggplant 2
Raisin 2
Fig 2
Bilberry 1
Horned melon 0.5
Medlar 0.3
[edit] Animal sources
Goats, like almost all animals, make their own vitamin C. An adult goat, weighing approx. 70 kg, will manufacture more than 13,000 mg of vitamin C per day in normal health, and levels manyfold higher when faced with stress.[155][156]
The overwhelming majority of species of animals and plants synthesise their own vitamin C, making some, but not all, animal products, sources of dietary vitamin C.
Vitamin C is most present in the liver and least present in the muscle. Since muscle provides the majority of meat consumed in the western human diet, animal products are not a reliable source of the vitamin. Vitamin C is present in mother's milk but, not present in raw cow's milk.[157] All excess vitamin C is disposed of through the urinary system.
The following table shows the relative abundance of vitamin C in various foods of animal origin, given in milligram of vitamin C per 100 grams of food:
Animal Source Amount
(mg / 100g)
Calf liver (raw) 36
Beef liver (raw) 31
Oysters (raw) 30
Cod roe (fried) 26
Pork liver (raw) 23
Lamb brain (boiled) 17
Chicken liver (fried) 13
Animal Source Amount
(mg / 100g)
Lamb liver (fried) 12
Calf adrenals (raw) 11[158]
Lamb heart (roast) 11
Lamb tongue (stewed) 6
Human milk (fresh) 4
Goat milk (fresh) 2
Camel milk (fresh) 5[159]
Cow milk (fresh) 2
[edit] Food preparation
Vitamin C chemically decomposes under certain conditions, many of which may occur during the cooking of food. Vitamin C concentrations in various food substances decrease with time in proportion to the temperature they are stored at[160] and cooking can reduce the Vitamin C content of vegetables by around 60% possibly partly due to increased enzymatic destruction as it may be more significant at sub-boiling temperatures.[161] Longer cooking times also add to this effect, as will copper food vessels, which catalyse the decomposition.[65]
Another cause of vitamin C being lost from food is leaching, where the water-soluble vitamin dissolves into the cooking water, which is later poured away and not consumed. However, vitamin C does not leach in all vegetables at the same rate; research shows broccoli seems to retain more than any other.[162] Research has also shown that fresh-cut fruits do not lose significant nutrients when stored in the refrigerator for a few days.[163]
[edit] Vitamin C supplements
Vitamin C is widely available in the form of tablets and powders. The Redoxon brand, launched in 1934 by Hoffmann-La Roche, was the first mass-produced synthetic vitamin C.
Vitamin C is the most widely taken dietary supplement.[164] It is available in caplets, tablets, capsules, drink mix packets, in multi-vitamin formulations, in multiple antioxidant formulations, and crystalline powder. Timed release versions are available, as are formulations containing bioflavonoids such as quercetin, hesperidin and rutin. Tablet and capsule sizes range from 25 mg to 1500 mg. Vitamin C (as ascorbic acid) crystals are typically available in bottles containing 300 g to 1 kg of powder (a teaspoon of vitamin C crystals equals 5,000 mg).
[edit] Industrial synthesis
Vitamin C is produced from glucose by two main routes. The Reichstein process, developed in the 1930s, uses a single pre-fermentation followed by a purely chemical route. The modern two-step fermentation process, originally developed in China in the 1960s, uses additional fermentation to replace part of the later chemical stages. Both processes yield approximately 60% vitamin C from the glucose feed.[165]
Research is underway at the Scottish Crop Research Institute in the interest of creating a strain of yeast that can synthesise vitamin C in a single fermentation step from galactose, a technology expected to reduce manufacturing costs considerably.[25]
World production of synthesised vitamin C is currently estimated at approximately 110,000 tonnes annually. Main producers have been BASF/Takeda, DSM, Merck and the China Pharmaceutical Group Ltd. of the People's Republic of China. China is slowly becoming the major world supplier as its prices undercut those of the US and European manufacturers.[166] By 2008 only the DSM plant in Scotland remained operational outside the strong price competition from China.[167] The world price of vitamin C rose sharply in 2008 partly as a result of rises in basic food prices but also in anticipation of a stoppage of the two Chinese plants, situated at Shijiazhuang near Beijing, as part of a general shutdown of polluting industry in China over the period of the Olympic games.[168] Five Chinese manufacturers met in 2010, among them Northeast Pharmaceutical Group and North China Pharmaceutical Group, and agreed to temporarily stop production in order to maintain prices.[169]
[edit] Food Fortification
Health Canada evaluated the effect of fortification of foods with abscorbate in the guidance document, Addition of Vitamins and Minerals to Food, 2005.[170] Health Canada categorized abscorbate as a ‘Risk Category A nutrients’. This means it is a nutrient for which an upper limit for intake is set but allows a wide margin of intake that has a narrow margin of safety but non-serious critical adverse effects. Health Canada recommended a minimum of 3 mg or 5% of RDI for the food to claim to be a source of Vitamin C, and maximum fortification of 12 mg (20% of RDI) to claim "Excellent Source."[170]

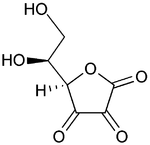
In enzymology, a L-ascorbate oxidase (EC 1.10.3.3) is an enzyme that catalyzes the chemical reaction2 L-ascorbate + O2 ↔ 2 dehydroascorbate + 2 H2O. Thus, the two substrates of this enzyme are L-ascorbate and O2, whereas its two products are dehydroascorbate and H2O. ascorbate oxidase
BalasHapus